Post-traumatic stress disorder and complex post-traumatic stress disorder are trauma-related conditions that may look similar on the surface, yet differ in ways that matter for understanding a person’s lived experience and support needs.
Trauma can disrupt a person’s sense of safety, predictability, and connection. While many people experience trauma without developing long-term psychological difficulties, others find that its effects persist and shape emotional responses, relationships, and self-understanding.
Post-traumatic stress disorder is a mental health condition that may develop after a person experiences or witnesses a traumatic event involving a threat to life, serious injury, or violation of bodily integrity [1].
This may include:
PTSD symptoms typically include [1,2]:
PTSD can significantly affect daily functioning, relationships, and a person’s felt sense of safety. For a diagnosis, symptoms must persist for more than one month and cause clinically significant distress or impairment [1].
Complex PTSD is a condition recognised in the International Classification of Diseases Eleventh Revision. It is related to PTSD but involves additional and distinct features [2,3].
Complex PTSD typically develops following repeated or prolonged interpersonal trauma, particularly in contexts where escape was limited or impossible. This trauma often occurs during formative developmental periods, though it can also arise in adulthood.
This may include:
For many people, these trauma responses are influenced by early relational experiences and are well conceptualised through attachment wounds , particularly when trauma occurs within close or caregiving relationships.
In addition to the core symptoms of PTSD, Complex PTSD is characterised by persistent difficulties across three broad areas [2,3]:
These difficulties may be experienced as:
These patterns reflect understandable adaptations to long-term threat and relational harm. They are not indicators of personal weakness or lack of effort.
Both PTSD and Complex PTSD are treatable. Effective treatment is typically individualised and paced, particularly for Complex PTSD, where establishing emotional safety and trust is foundational [4,5].
Evidence-based approaches include:
Rather than erasing traumatic experiences, therapy aims to reduce their ongoing impact, strengthen emotional regulation, and support greater flexibility, agency, and quality of life.
Psychologists often work collaboratively with general practitioners and psychiatrists to provide coordinated, ethical, and person-centred care for people experiencing PTSD or Complex PTSD.
Psychological therapy is usually the first-line treatment [4]. Medication may be considered when symptoms remain severe despite therapy, when there are co-occurring conditions such as depression or anxiety, or when a person is temporarily unable or unwilling to engage in therapy.
Medication does not process trauma directly, but it may reduce symptom intensity and create greater capacity to engage in psychological treatment.
If you would like support for PTSD or Complex PTSD, you are welcome to arrange an appointment.
https://hennessyclinicalpsychology.com/contact/
What is the difference between PTSD and Complex PTSD?
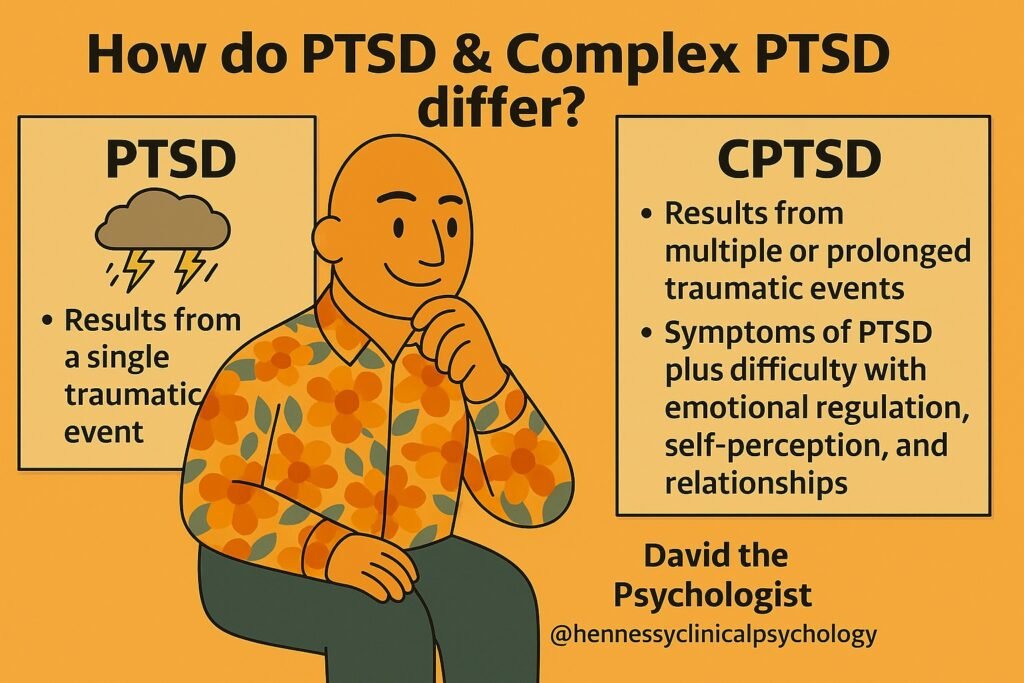
PTSD commonly develops after a single traumatic event, whereas Complex PTSD usually develops following prolonged or repeated interpersonal trauma. Complex PTSD includes additional difficulties with emotional regulation, sense of self, and relationships, which influence how therapy is paced and structured.
Is Complex PTSD recognised as a diagnosis?
Yes. Complex PTSD is formally recognised in the International Classification of Diseases Eleventh Revision and is supported by a strong international evidence base.
Can childhood trauma lead to Complex PTSD in adulthood?
Yes. Prolonged trauma during childhood, particularly within caregiving relationships, can contribute to patterns of emotional regulation difficulty, shame, and relational insecurity that persist into adulthood.
How is Complex PTSD treated differently from PTSD?
While both conditions benefit from trauma-focused therapy, treatment for Complex PTSD often places greater emphasis on safety, stabilisation, emotional regulation, and relational trust before or alongside trauma processing.
Do I need a formal diagnosis to seek help?
No. Therapy focuses on your lived experience and support needs, not just diagnostic labels.
At Hennessy Clinical Psychology in Varsity Lakes, we offer compassionate, evidence-based, trauma-informed psychological support. Whether you are dealing with a single traumatic event or the long-term impact of Complex PTSD, therapy is approached collaboratively and at a pace that prioritises safety, understanding, and dignity.