What is Adult ADHD?
By David Hennessy, Clinical Psychologist
Adult Attention Deficit Hyperactivity Disorder (ADHD) is a neurodevelopmental condition characterised by persistent patterns of inattention, impulsivity, and hyperactivity that interfere significantly with everyday functioning and quality of life. Often misunderstood or overlooked, ADHD can profoundly impact adults and influence relationships, career progress, and emotional wellbeing.
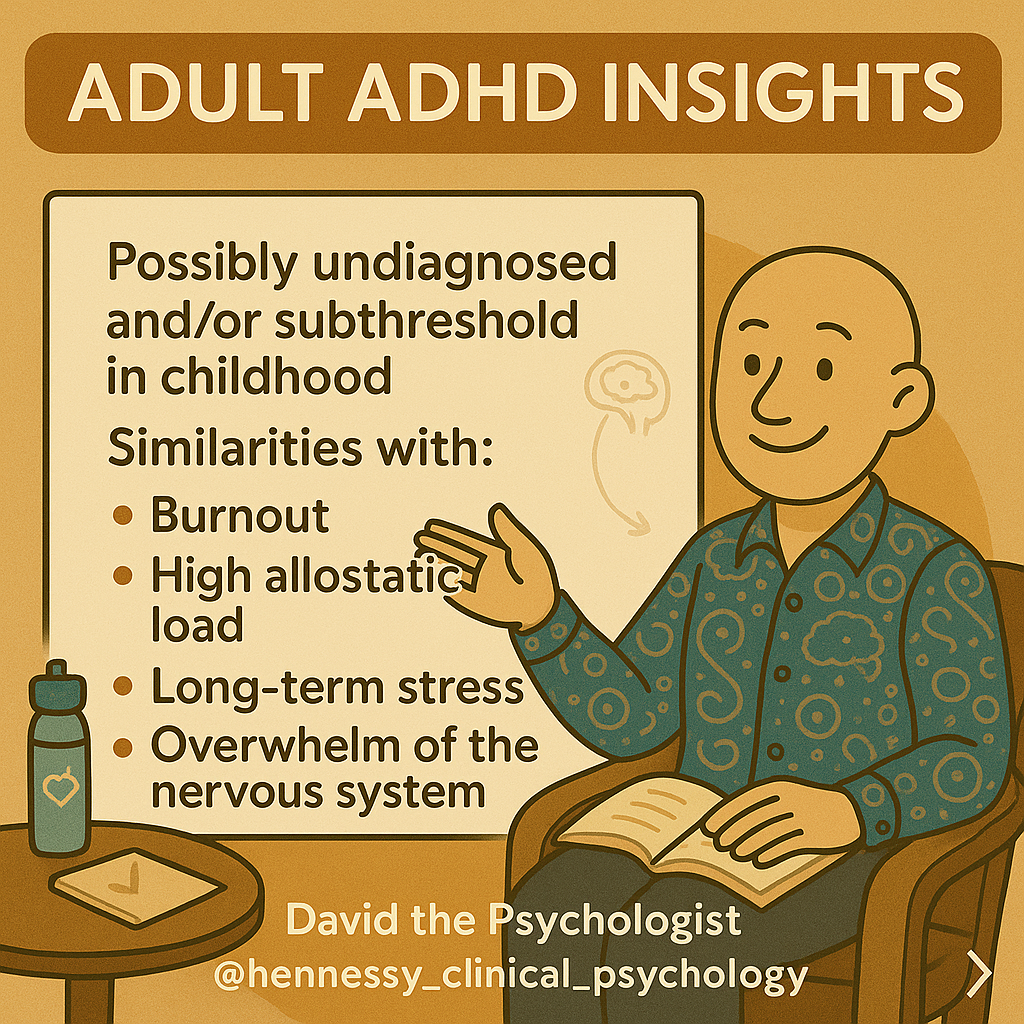
Possibly Undiagnosed or Subthreshold in Childhood
Many adults with ADHD were never diagnosed during childhood or had symptoms that were not pronounced enough to attract clinical attention. Childhood ADHD symptoms may be subtle, resulting in adults who grow up feeling chronically overwhelmed, stressed, or misunderstood without understanding why.
Similarities to Trauma Syndrome and Burnout
The lived experience of adults with undiagnosed or subthreshold ADHD can share similarities with trauma syndromes and burnout. These patterns often include:
- Chronic stress: Ongoing efforts to manage ADHD symptoms can contribute to emotional exhaustion and reduced resilience.
- High allostatic load: The cumulative effect of stress on the body is often elevated, similar to prolonged trauma or long-term pressure.
- Overwhelmed nervous system: Many adults describe a constant sense of overload, mirroring emotional and physiological patterns seen in trauma-related presentations.
Recognising Adult ADHD
- Difficulty concentrating or maintaining focus
- Persistent procrastination and organisational challenges
- Frequent mood shifts and emotional dysregulation
- Restlessness or difficulty relaxing
- Impulsive behaviours and decisions
Hope and Management
Identifying adult ADHD can be life-changing. Many people describe a deep sense of relief when lifelong challenges start to make sense. With the right support, such as cognitive behavioural therapy, structured lifestyle strategies, and sometimes medication, people often experience meaningful improvements in functioning, emotional balance, and confidence.
References
- Barkley, R. A. (1997). Behavioural inhibition, sustained attention, and executive functions. Psychological Bulletin, 121(1), 65 to 94. https://doi.org/10.1037/0033-2909.121.1.65
- McEwen, B. S., & Stellar, E. (1993). Stress and the individual. Archives of Internal Medicine, 153(18), 2093 to 2101. https://doi.org/10.1001/archinte.1993.00410180039004
- Arnsten, A. F. T. (2009). Stress signalling pathways and prefrontal cortex function. Nature Reviews Neuroscience, 10(6), 410 to 422. https://doi.org/10.1038/nrn2648
- van der Kolk, B. (2014). The Body Keeps the Score. Viking.
- Faraone, S. V. et al. (2021). ADHD International Consensus Statement. Neuroscience and Biobehavioral Reviews, 128, 789 to 818. https://doi.org/10.1016/j.neubiorev.2021.01.022
- Sibley, M. H. et al. (2022). ADHD in adulthood. Current Opinion in Psychiatry, 35(5), 297 to 304. https://doi.org/10.1097/YCO.0000000000000811
- Australian ADHD Professionals Association. (2022). Australian Evidence-Based Clinical Practice Guideline for ADHD. https://adhdguidelines.org.au